Guide for primary care will optimize the care process for people with anxiety and depression
The MSP presented a series of recommendations to improve the care process for people with anxiety and depression in the National Integrated Health System. The document organizes the demand for care, reinforces the first level to avoid the referral of the person to a psychiatrist and takes advantage of the resources of licensed nurses. “These are concrete actions in mental health,” said Undersecretary José Satdjian.
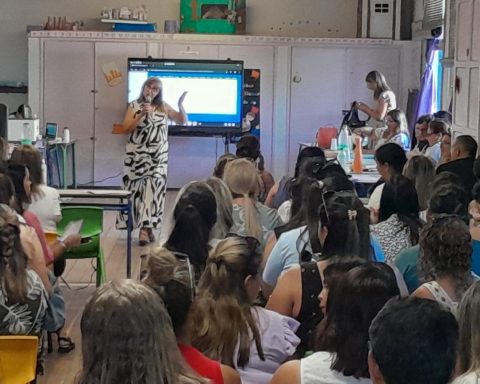
The guide was presented yesterday morning, Tuesday 27, at the headquarters of the Ministry of Public Health (MSP). Also participating were the Director and Deputy Director General of Health, Adriana Alfonso and Jaqueline Coronato, respectively, and the Director of the Mental Health Program, Alejandra Moreira.
Satdijan stressed that the guide represents another link in the chain of actions and work carried out in this period in the area of mental health, under the premise of respect and responsibility.
“After the pandemic, we put the issue of mental health on the table, working with WHO parameters, which reported a 30% increase in consultations, so it was decided to deepen care and break the paradigm that mental health would not be discussed,” she said. She added: “Nowadays, there is more and more talk and responsible work is being done on proposals accompanied by actions.”
The official explained that the guide regulates the demand for care, in addition to reinforcing and supporting the first level to avoid the referral of the person to a psychiatrist, which allows for faster assistance. It also takes advantage of the resources of nursing graduates, who have training and experience so that care is provided in a humanized manner, he added.
The guide data
The guide contains a series of recommendations, such as strengthening human resources, telemedicine and digital interventions; intervening together with a community representative, implementing tiered care models, assessing demand and maintaining continuity of care.
The objectives of the document are to organize demand, support services and professionals in decision-making, establish a clear care process, reduce variability in clinical practice, integrate notions of humanization and shared decision-making, prioritize an approach based on the primary health care strategy, with emphasis on the first level of care and evidence-based practices, and prevent unnecessary medicalization and psychologization of human suffering.
Interventions are carried out in three steps: the first consists of prioritising the use of non-pharmacological human resources as part of the clinical interview, providing guidance to the person and family members and emotional references. The second involves the psychotherapeutic and psychosocial approach and the third, includes pharmacological treatment and psychological interventions of greater intensity and duration.