This week, a new disease put the world’s health authorities on alert. As if coronavirus and monkeypox weren’t enough, now countries might have to worry about Marburg virus.a hemorrhagic fever almost as deadly as Ebola.
The new public health alert is given because Ghana detected last week two suspected cases of Marburg virus.
What is Marburg virus?
The Marburg virus (MVD) It is a hemorrhagic fever almost as deadly as Ebola. MVD was first identified in 1967 after simultaneous outbreaks in Marburg and Frankfurt (Germany) and in Belgrade (Serbia).
You may be interested in: Carolina Corcho, MinSalud of Petro, talks about her proposal to eliminate the EPS in Colombia
The lethality of Marburg virus disease (MVD), which is caused by the virus that bears this name, it is up to 88%, but could be much lower if patients were properly cared for.
Although Marburg and Ebola viruses are different viruses, both belong to the Filoviridae family and cause diseases with similar clinical characteristics. Both are rare, but case fatality rates from their outbreaks can be high.
The WHO reports that there were two major outbreaks occurring simultaneously in Marburg and Frankfurt (Germany) and in Belgrade (Serbia) in 1967 allowed the disease to be identified for the first time.
These outbreaks were associated with laboratory work with African green monkeys (Cercopithecus aethiops) imported from Uganda. Subsequently, outbreaks and sporadic cases have been reported in Angola, Kenya, the Democratic Republic of the Congo, South Africa (in a person who had recently traveled to Zimbabwe), and Uganda.
In 2008, two independent cases were reported in travelers who had visited a cave inhabited by colonies of bats. Rousettus in Uganda.
Transmission
Initially, human infection by MVD is due to prolonged stay in mines or caves inhabited by colonies of bats. Rousettus.
Person-to-person transmission occurs by direct contact of broken skin or mucous membranes with blood, secretions, organs or other bodily fluids from infected persons, as well as surfaces and materials contaminated with such fluids, such as personal clothing or bedding.
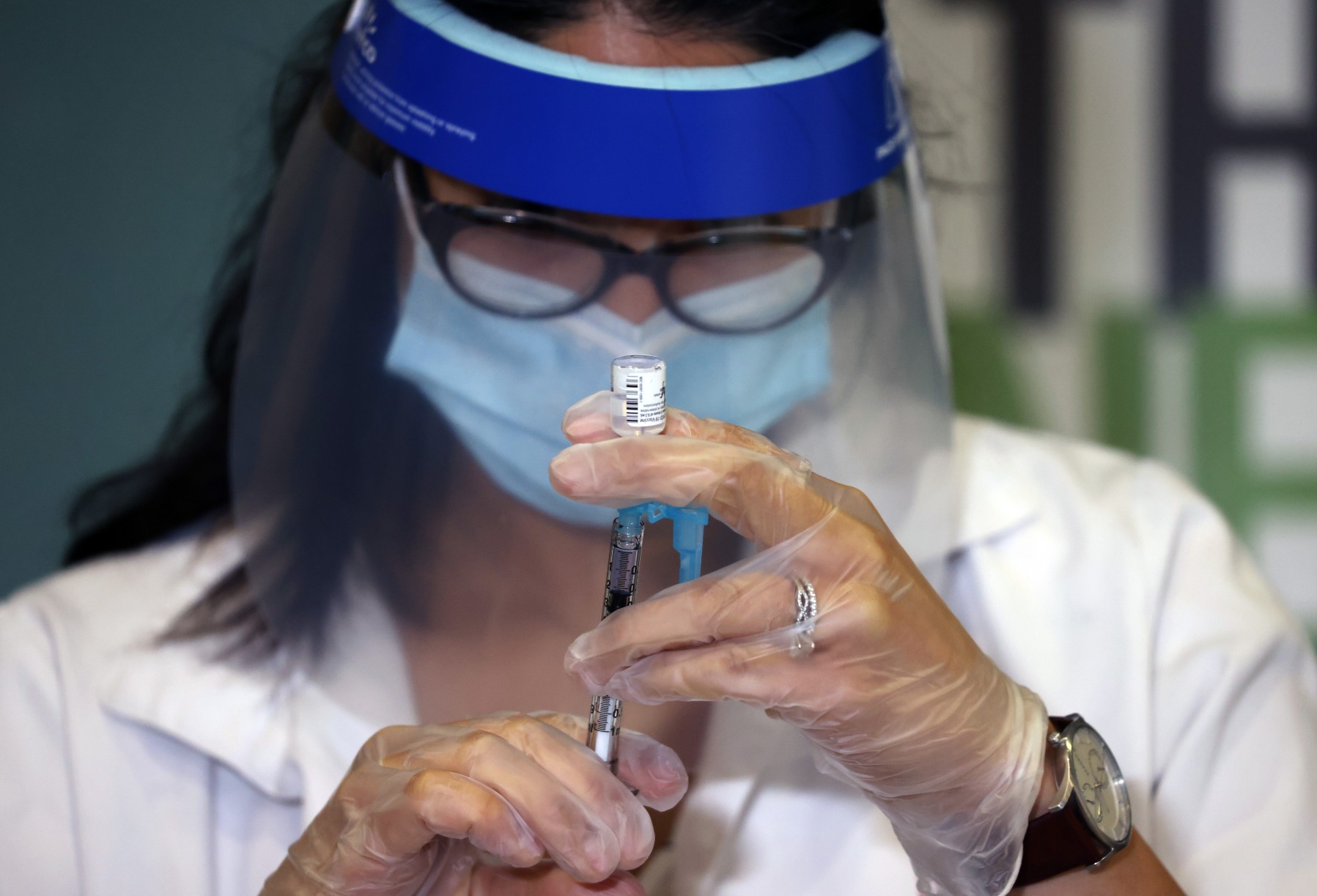
Cases of transmission to healthcare personnel caring for patients with E.Suspected or confirmed MV, through close contact without proper infection control precautions. Transmission through contaminated injection equipment or needle sticks is associated with increased severity of illness, faster worsening, and possibly a higher case fatality rate.
This transmission can also be given in funeral ceremonies in which the mourners have direct contact with the body of the deceased. Infectivity persists as long as there is virus in the blood.
Symptoms
The incubation period (ie the interval between infection and onset of symptoms) ranges from 2 to 21 days.
MVS begins abruptly, with high fever, intense headache and great malaise, as well as frequent muscle pain. On the third day, intense watery diarrhoea, abdominal pain and cramps, nausea and vomiting may appear. Diarrhea may persist for a week.
In this phase, it has been described that patients have a “ghost appearance” due to sunken eyes, facial expressionlessness, and extreme lethargy. In the European outbreak in 1967, most patients developed a nonpruritic rash 2 to 7 days after the onset of symptoms.
Many patients have severe bleeding manifestations within 5 to 7 days, and fatal cases usually have some form of bleeding, often in multiple organs. The presence of fresh blood in vomit and feces is often accompanied by bleeding from the nose, gums, and vagina.
You may be interested in: Video: They reveal shocking images of what a silicone breast looks like after 30 years
Spontaneous bleeding at venipuncture sites where fluids are given or blood samples are drawn can be especially troublesome. During the severe phase of the disease, patients have a persistently high fever. Central nervous system involvement can produce confusion, irritability, and aggressiveness. Occasional cases of orchitis (inflammation of one or both testicles) have also been described in the late phase of the disease (15 days after onset).
In fatal cases, death usually occurs 8 or 9 days after the onset of symptoms and is usually preceded by significant blood loss and shock.