“Silence kills, talking about tuberculosis and HIV will save lives,” Nelson Mandela.
Recently I participated in the eighth edition of the High Level Forum on Innovation for the Mexican Legislative Power, organized by the Wilson Center Institute and the Idea Foundation. In panel four, on learning and use of success cases, HIV management was discussed nationally and internationally, the topic on which I want to reflect.
The current HIV situation in Mexico. It is estimated that in Mexico there are 370,000 people living with the human immunodeficiency virus (HIV). Alarmingly, 28% do not know their condition, leaving without diagnosis, treatment, or control to avoid their silent propagation. By 2030, Mexico has proposed ambitious goals: 95% know their serological status (currently 73%); 95% of patients in antiretroviral therapy (currently 85%) and 95% with undetectable viral load (currently 93%)
The epidemiological bulletin of the last week of 2024 reported 17,953 confirmed cases, 9.4% more than in 2023. 85% were men and 15% women. The distribution by clinical stages was: Stadium I: 7,718 men and 1,493 women. Stage II: 2,190 men and 351 women. Stage III: 3,280 men and 540 women. Stage IV: 2,007 men and 374 women.
The resurgence of tuberculosis. At the same time, tuberculosis is resurfaceing strongly. The epidemiological bulletin of week 52 reported 20,289 new cases of respiratory tuberculosis and 517 tuberculous meningitis. As a doctor and researcher, I have witnessed how this bacterium has evolved, becoming more resistant and finding a mortal ally in HIV. In week 2 of 2025, 284 new cases of respiratory tuberculosis were reported, exceeding the historical median. Oblutingly, 17 cases of tuberculous meningitis were recorded, a serious form of the disease.
A dangerous combination. HIV coexistence and tuberculosis is particularly alarming. In the same week 79 new cases of HIV were reported, reflecting an upward trend. HIV weakens the immune system, facilitating the development of active tuberculosis and complicating its treatment. The scenario is aggravated by the migratory flows that go through Mexico. Thousands of people travel in precarious conditions, promoting the spread of diseases. This movement hinders monitoring and treatment, increasing the risk of developing resistant strains.
Imagine Maria, a young migrant who crosses our country. Without knowing it, it carries with it the bacillus of tuberculosis, acquired in conditions of overcrowding during its journey. Upon arriving in a border city, he meets Juan, a young man who lives with HIV but still doesn’t know. His casual encounter triggers a chain of infections that puts the community in check and the country sooner rather than later. This fictitious story illustrates an alarming reality because we must take urgent actions on several fronts:
- Research and development of new antibiotics: the article of Saukkonen et al. Published by the American thoracic society highlights the urgent need to develop more effective antibiotics against resistant strains. For HIV, it is required to expand immediate treatment and combined prevention.
- Strengthening epidemiological surveillance: We must improve early detection and monitoring of cases, especially in high mobility areas. For HIV, implement accessible self -tests and integrated tests in mobile centers.
- Technological innovation: It is crucial to have a unified electronic file between health subsystems, monitoring platforms and telemedicine tools.
- Comprehensive care to vulnerable populations: Implement programs that simultaneously address the prevention and treatment of tuberculosis and HIV.
- Education and awareness: Inform the health personnel and the population about risks and symptoms to facilitate timely detection.
- International cooperation: collaborate closely with other countries to share information and coordinate strategies.
- Crucial role of the Legislative Power: Update the regulatory framework, eliminate barriers such as discrimination, and assign budget for prevention, diagnosis and research.
Returning to our fictitious history, let’s imagine a different outcome: Maria is detected in a health control post when entering the country. Receive proper treatment and monitoring. Juan, on the other hand, accesses an HIV test and begins early antiretroviral therapy. Both recover and become health promoters in their community. This alternative scenario is possible if we act with decision and vision of the future.
A call to action. Tuberculosis and HIV are not only medical problems, but challenges that require comprehensive approach including social, economic and political aspects. I invite my legislators, the medical community and society in general to join efforts to face this threat. Just working together we can write a hopeful ending for this story that involves thousands of Mexicans and migrants. Public health knows no borders, and our commitment must be equally broad and supportive.
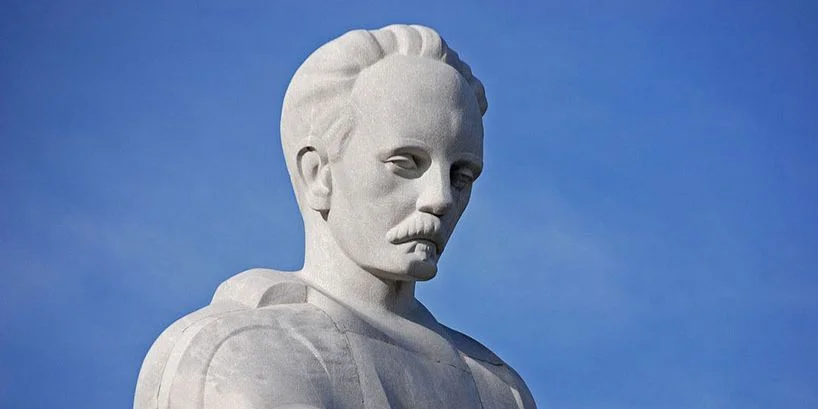
* Éctor Jaime Ramírez Barba (www.lectorjaime.mx) is a specialist in general surgery, public health certificate, doctorate in health sciences and public administration. He is a legislator and defender of the public health of Mexico, reelected deputy of the Parliamentary Group of the PAN in the LXVI Legislature.