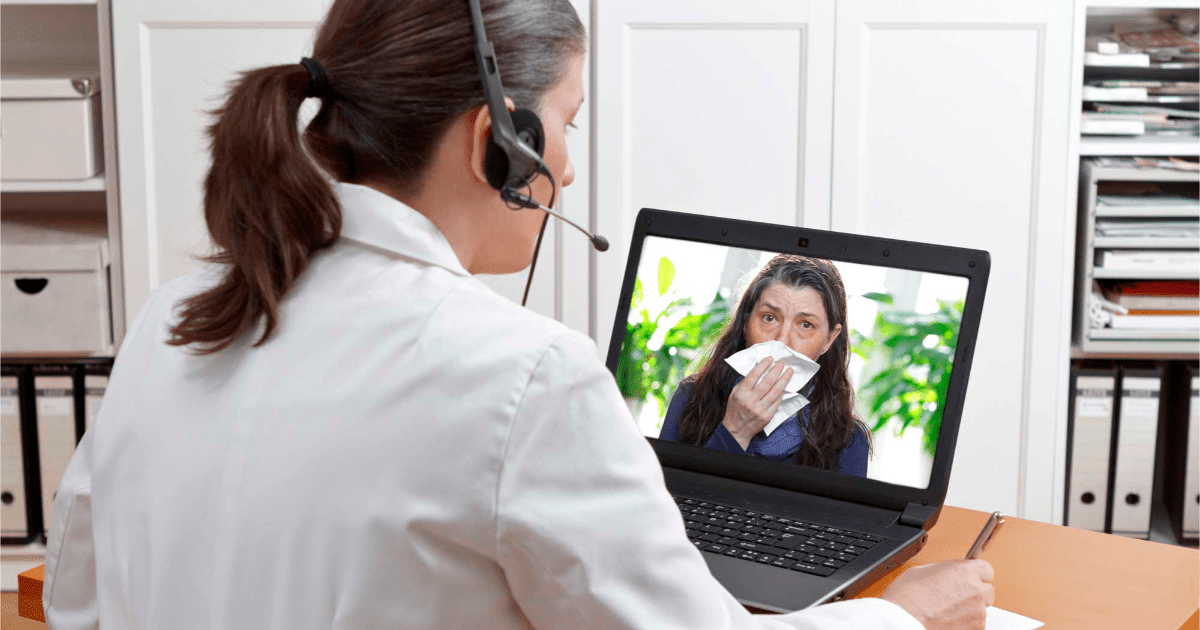
When the epidemiological traffic light was declared red for the first time, due to the covid-19 pandemic in Mexico City, Dr. Raquel Faradji, director of the EnDi Clinic, had five days to return from a risk area, at that time not much was known about the transmissions, nor about the clear measures to avoid contagion, but what was a fact was that it was not possible to put at risk patients in face-to-face consultation. “It was adapting to the situation. It was Monday, March 16, 2020, the next day I had a full consultation. What was done immediately in the clinic was a decree that was sent by mail, a blog was made where the information was posted, all the patients were notified and as of February 17, the consultations went to telemedicine”.
From one day to the next everything changed, from then on the work went in different directions, the specialist in internal medicine, endocrinology, diabetes and metabolism talks. First, to keep the patient well informed of what was going to happen to her and to schedule her appointments appropriately; second, that the doctor managed to have all the information that is required about the patient.
This translates into the arrival of information, its integration and prescribing with clear instructions. He explains that in reality the structure of the consultation is very similar to the normal consultation, but with the method known as PSOA, that is: Patients and their medications, to be able to recognize if something is causing an adverse effect and that is what originates the consultation of the patient; the subjective, referring to the patient’s problems and concerns; the objective, where the vital signs and some physical examination are seen; and laboratory analysis, which are key to treatment and control.
The specialist assures that for all this to happen, smartphones have been a key element, “as a doctor you now have your platform, the electronic file, the prescription that can be sent from the file to a group of WhatsApp. In the ideal world, it would be that everything was in the same electronic file, since in reality diseases are treated in a multidisciplinary way”.
For Dr. Faradji, there will come a time when everything can be seen in the same place, where the patient cooperates with informative data, and at the same time can see their analysis, which is operable and easy to use. “For now, there are still many screens that are used, on the one hand, Zoom, the electronic file, the meters, the laboratories, the PDFs, everything is separate.”
Digital Health Law
Dr. Faradji, who participated in the fourth edition of the Novo Nordisk Leaders Summitheld from February 25 to 27, for the telemedicine regulation will be an important issue in the coming years, since “it is here to stay”.
Although today some applications are regulated by health authorities, be it the Federal Commission for the Protection against Sanitary Risks (Cofepris), in Mexico, or the Food and Drug Administration (FDA) in the United States, there are also very good projects that are not necessarily approved by these agencies, therefore a more robust work is required.
This is what is being promoted by Dr. Éctor Jaime Ramírez Barba in the Chamber of Deputies, to have the right to remote consultation, that prescriptions be filled electronically, to have an electronic file regardless of the institution and telediagnosis. This initiative arises from the project of the global strategy on digital health of the World Health Organization 2021-2025. Here it is pointed out that digital health must be part of health priorities and benefit people in an ethical, safe, reliable, equitable and sustainable way.
Raquel Faradji, director of the EnDi Clinic. Photo EE: Courtesy
Dr. Faradji believes that technology advances faster than the Law, that is why we are going to need a Law that is flexible enough to be able to incorporate the constant evolution of telemedicine. “That it does not become stagnant saying that, for example, this or that electronic file is forced to be used, these are going to evolve and the information is going to be integrated more easily, then you have to allow the new technologies to be accepted in the legislation”
He said that one of the fundamental points will be the confidentiality and privacy of the patient, “that the security of the transfer of information be the safest and that sensitive information is not leaked to a place where it should not be. If that is done, it is about meeting the highest quality standards and research can be done to show that this has results, we could soon achieve a Digital Health Law that works.”
The specialist concludes that the more legality and legal framework, the better, because an empowered patient can study and decide whether or not to use a tool, but for another who has not achieved that empowerment, it is much better to review stamps or certifications that give him validity and support to things.
technology in diabetes
In the voice of Dr. Faradji, in many cases the telemedicine it came from one day to the next, and although today we are returning to face-to-face consultations, the reality is that there were people who turned their health care around for the better.
For example, some diabetes patients now use insulin pumps that enable fully digital work. For a patient with diabetes, glucose monitoring is the compass to know whether or not they are in the right place, for type 1 diabetes, monitoring is at least 4 and up to 10 times a day. “This is necessary to have metabolic control and reduce the probability of having long-term chronic complications.” A recent article also came out associating the use of continuous glucose monitoring in patients with type 2 diabetes with lower mortality.
He said that during the pandemic interesting things happened for these patients. “We had people who could not lower glycosylated hemoglobin below 9% and managed to reach 7% (adequate levels) during the pandemic and virtually (…) now patients ask me if they really have to go to a consultation. There are reviews that by their nature must be face-to-face, but for example, in the case of patients with type 1 diabetes, who rigorously require insulin, they come once a year for their face-to-face consultation and the rest are virtual. This has come to transform the way in which medical consultation is given”.
kg